Cancer that is detected early is smaller and more easily treated.
The American Cancer Society tells us on its website, “Getting regular screening tests is the most reliable way to find breast cancer early.” However, the more aggressive breast tumors tend not to be diagnosed by mammogram but by palpation (feel).
From the New England Journal of Medicine in January 2017:
Screening mammography increases the incidence rates of nonlethal cancers (i.e., those with favorable biologic characteristics) but has little effect in reducing incidence rates of potentially lethal cancers (i.e., those with aggressive phenotypes).
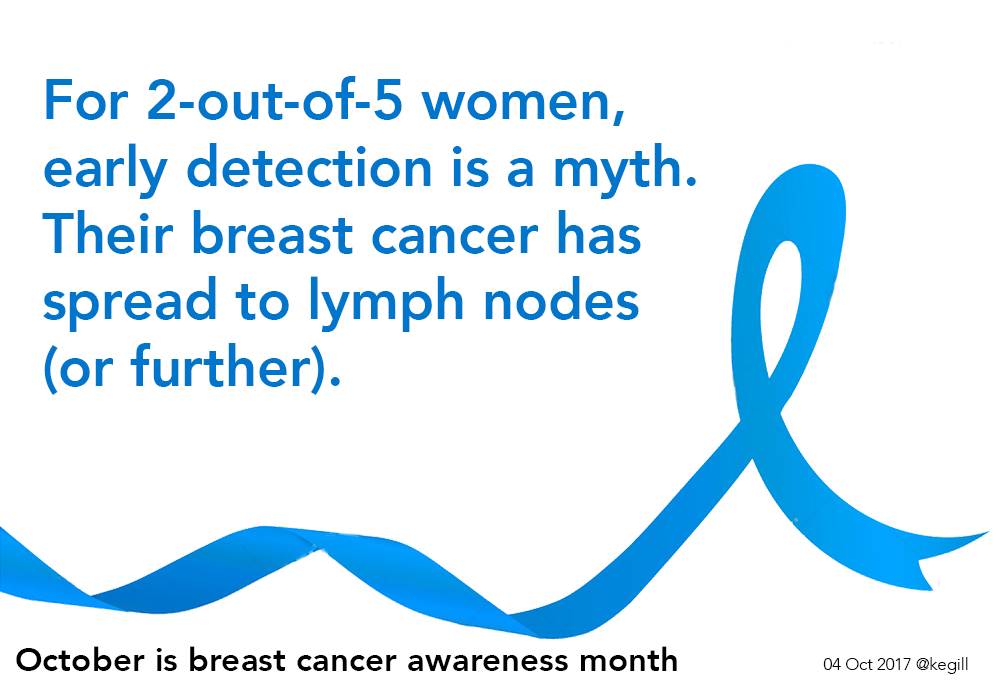
For 3-in-10 women, their breast cancer has spread to their lymph nodes at diagnosis. Sometimes this is aggressive ductal cancer (IDC); often it is lobular cancer (ILC), which is difficult to detect. For six percent, their breast cancer is not diagnosed until it has spread to other parts of the body (metastasized).
Therefore, despite the focus on early detection, only 6-in-10 cases of breast cancer are diagnosed as truly local to the breast. Some of these cancers, ductal carcinoma in situ (DCIS), have not escaped the confines of the breast ducts to affect other breast tissue. Since 1975, there has been a 324% increase in the rate of DCIS cases diagnosed.

Although tumor size is used to determine cancer stage, it is not necessarily a proxy for risk. A larger cancer can be slow growing; a smaller cancer can be fast growing. And it is ductal cancers that form a mass that is correlative to the Mayo image above.
Other factors that determine risk-to-life include
- whether or not the cancer has spread to lymph nodes (N+/N-)
- how fast the cancer is growing (Ki-67)
- how mutated the cancer cells appear to be (grade)
- estrogen or progesterone receptor positive (ER+/PR+) or negative (ER-/PR-)
- HER2 receptor positive (HER2+) or negative (HER2-)
- the age of the woman or man when diagnosed with breast cancer.
As a general statement, tumors that are ER+ and/or PR+ are slightly slower growing and have a slightly better prognosis than tumors that are ER- and/or PR-. HER2+ tumors tend to be more aggressive but they can be treated with a HER2-targeted therapy.
In a study of 50,399 patients with lobular and ductal cancer, 49% of the patients with ductal cancer had tumors larger than 2 cm at diagnosis. For lobular cancer, 54% of the patients had tumors larger than 2 cm at diagnosis and 14% had tumors larger than 5 cm (compared to 9% for ductal).
From the Dr. Susan Love Research Foundation:
Because lobular cancers elicit less scarring, they tend to grow to larger sizes (average 5 cm) than ductal carcinoma (average 2 cm) before they are detected.
Lobular cancer is hard to detect
Invasive lobular cancer (ILC) often fails to form a distinct tumor that can be easily seen on a mammogram or felt by palpation. Instead, the cancer cells line up single file and sometimes create webs. Thus ILC is difficult to detect:
The low density of tumor cells and lack of desmoplastic stromal reaction in ILC account for the difficulty in its detection on physical examination, mammography, and even gross pathologic evaluation. Mammograms have been found to have a low sensitivity (57-79%) in detecting ILC, with up to 30% of cases not visualized at all on mammography, and 35% of lesions only visible on one view.
Finally, from the January 2017 New England Journal of Medicine, H. Gilbert Welch, M.D., Dartmouth, and Philip C. Prorok, PhD, National Cancer Institute:
…the biologic heterogeneity of what we call breast cancer conspires to limit the benefit of screening…
Does this mean that women who are at an elevated risk of breast cancer should forego mammography? No. (They might need to have MRIs, too, although they are not perfect either.)
But it does mean that we are overly reliant on a system that does not seem to be making a dent in early detection of more aggressive breast cancer. The shift from film to zeros-and-ones has not resulted in our being able to better detect lobular cancer or later stage ductal cancer.
Read the series
October 1
October 2
October 3
October 4
The author, Kathy Gill, was diagnosed with invasive lobular carcinoma in June 2017.
Known for gnawing at complex questions like a terrier with a bone. Digital evangelist, writer, teacher. Transplanted Southerner; teach newbies to ride motorcycles. @kegill (Twitter and Mastodon.social); wiredpen.com